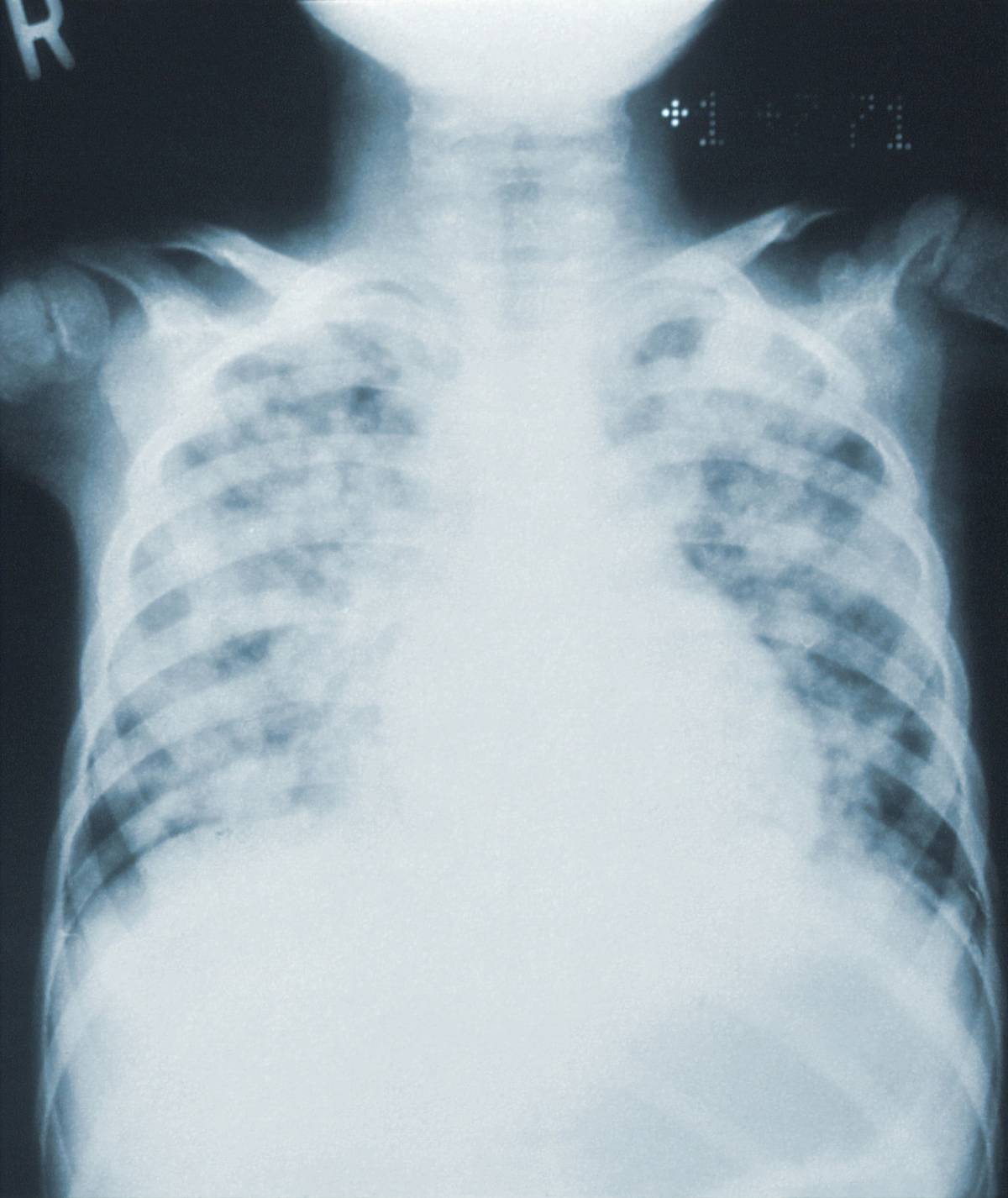
Pneumonia is an infection in the lungs. It can be caused by a variety of different pathogens, but pneumonia most commonly occurs as a complication from influenza or other viral respiratory infections. Antibiotics are often used to treat pneumonia, and urgent care may be necessary if the pneumonia symptoms are severe.
The topic of pneumonia and antibiotic treatment has been a popular subject in recent years. This is mainly due to the fact that the illness, while perceived to be insignificant, can cause significant damage to the human body and even death if it’s not properly treated.
As you will find out, antibiotics and urgent care are paramount when it pertains to containing the illness of pneumonia and curbing its effects.
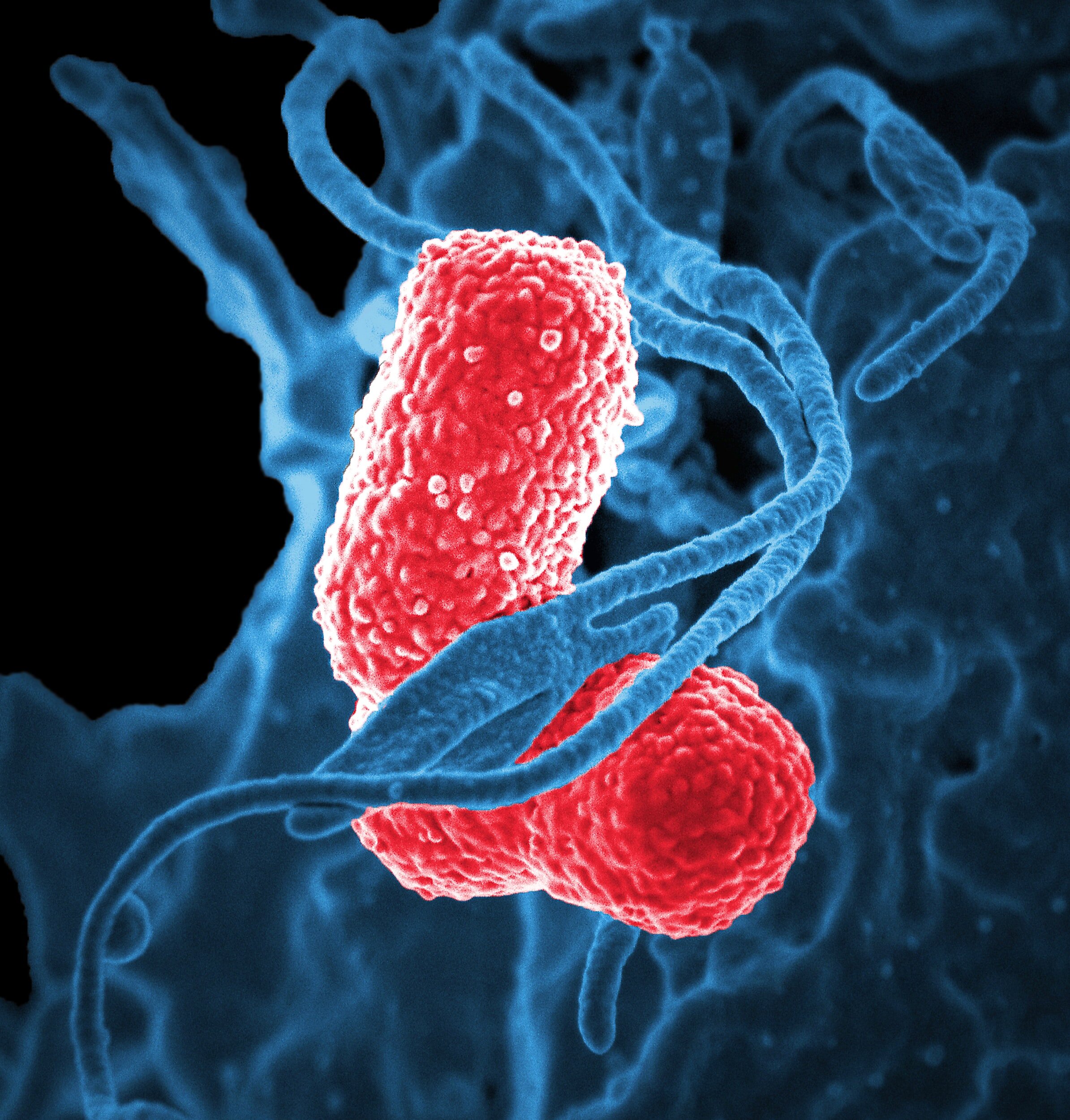
What are the Pathogens That Cause Pneumonia?
The typical pathogens that cause pneumonia are:
-
Streptococcus pneumonia
-
Haemophilus influenzae
Other pathogens include:
-
Mycoplasma pneumonia
-
Legionella pneumophila
-
Chlamydia pneumoniae
Who is at Risk of the Severe Effects of Pneumonia?
Extensive treatment for pneumonia is given to individuals for:
-
Older patients
-
Smokers
-
Those with comorbidities (CHF/liver or kidney disease/DM/EtOH) and/or recent antibiotic use.
The Dilemma with Viral Pathogens
While viral, infectious pathogens are the leading cause of pneumonia, there are modern guidelines that dictate the empirical treatment of this illness on a case-by-case basis.
The reason why is because there are currently no tests that can confirm whether or not a patient’s illness was caused solely by a virus. In fact, some patients’ illnesses may have been caused by bacterial coinfection.
As a result, clinicians use a formula called CURB-65 to determine the severity of pneumonia severity and the need for hospitalization:

The New Approach to Pneumonia and Antibiotics
MRSA and aeruginosa are two organisms that can result in more severe effects of pneumonia. These risks can actually take place after prior antibiotic and respiratory treatment within 90 days.
As such, clinicians will treat both stains until a confirmed positive hospital sputum test. The prior method of conducting this treatment has its disadvantages, mainly leading to the possible recurrence of pneumonia after a hospital sputum test.
The traditional way of treating pneumonia, known as macrolide monotherapy, has fallen under scrutiny because of this risk. This treatment shouldn’t be used if the patient’s resistance to pneumococcus is greater than 25%.
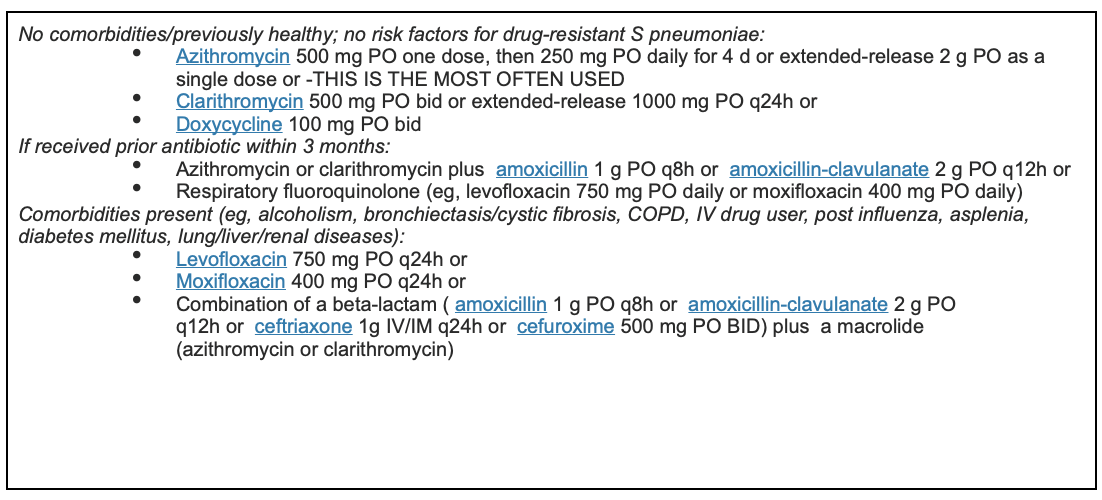
Currently, the average rate of resistance to pneumococcus is 30%.
Effective antibodies used to combat pneumonia are:
-
Xenleta (Lefamulin monotherapy) — This treatment is for patients who are resistant to beta-lactams who want to avoid the negative effects of fluoroquinolones (e.g. h/o tendon rupture).
-
Delafloxacin (Baxdela) — This treatment option is used by adults who contracted pneumonia due to S pneumoniae, MSSA, selected gram-negative pathogens (Klebsiella pneumoniae, Escherichia coli, P aeruginosa, H influenzae, Haemophilus parainfluenzae), and atypical microorganisms (C pneumoniae, L pneumophila, M pneumoniae).
What is the Duration of Antibiotic Therapy?
-
Most ambulatory patients with CAP for five days.
-
Azithromycin (because of its long half-life) at a dose of 500 mg daily can usually be treated for three days.
-
Patients should be afebrile for ≥48 hours and clinically stable before therapy is discontinued. When this is achieved, the persistence of other symptoms (eg, dyspnea, cough) is not an indication to extend the course of antibiotic therapy.
-
Several meta-analyses evaluating patients with mild to moderate CAP found comparable clinical outcomes with less than seven days compared with more than seven days of antimicrobial therapy.
Wikipedia reference: β-lactam antibiotics (beta-lactam antibiotics) are antibiotics that contain a beta-lactam ring in their molecular structure. This includes penicillin derivatives (penams), cephalosporins and cephamycins (cephems), monobactams, carbapenems[1] and carbacephems.[2] Most β-lactam antibiotics work by inhibiting cell wall biosynthesis in the bacterial organism and are the most widely used group of antibiotics. Until 2003, when measured by sales, more than half of all commercially available antibiotics in use were β-lactam compounds.[3] The first β-lactam antibiotic discovered, penicillin, was isolated from antibiotic discovered, penicillin, was isolated from a rare variant of Penicillium notatum (since renamed Penicillium chrysogenum).







